The Hot Night Skin Edit
Sleeping through an Australian summer after 40
Why summer nights hit differently after 40
Hot flushes and night sweats are two of the most common symptoms of menopause, affecting up to three quarters of women, and they can last for years for some.
At the same time, sleep disturbance becomes more frequent across the menopause transition. Large studies suggest that between 40 and 69 percent of women report poor sleep or insomnia during this stage of life.
When you combine those hormonal changes with an Australian summer, you get a perfect storm:
- Nights that do not cool down enough for your body to reset
- Bedding and sleepwear that suddenly feel like cling film
- A nervous system that is already more sensitive to heat, noise and stress
If you are lying awake at 3 am, damp and irritated in every sense of the word, it is not you being dramatic. It is biology, weather and life stage colliding.
This Skin Edit is about making those nights more liveable – skin, sleep and nervous system together – without promising miracle fixes.
What is actually happening to your body at night
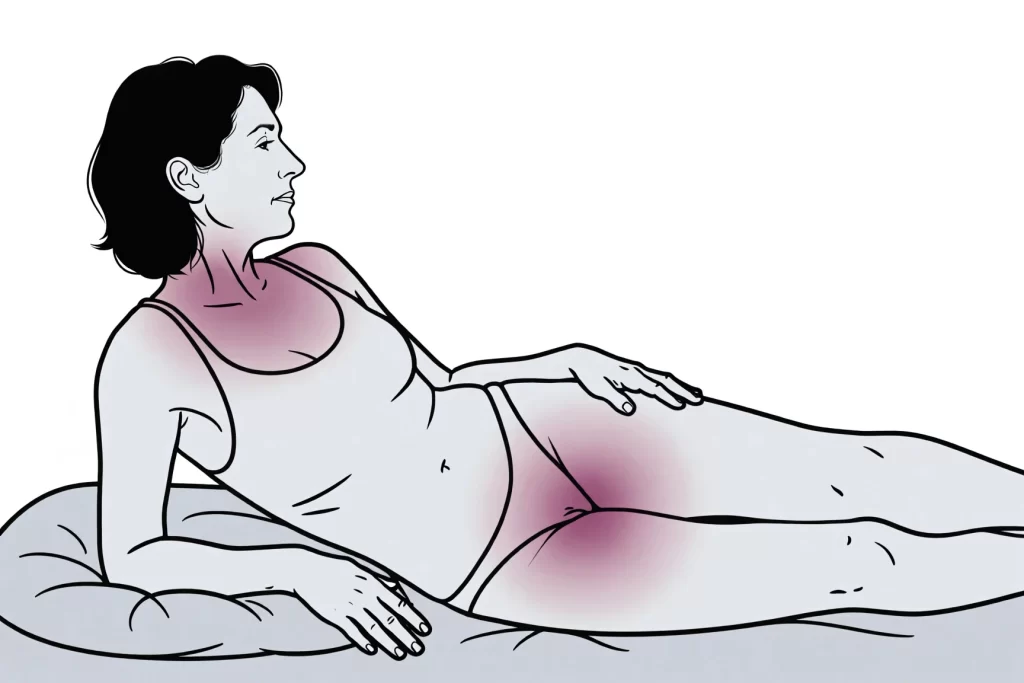
During peri and postmenopause, fluctuating and then lower oestrogen affect the part of the brain that regulates temperature. Hot flushes and night sweats are vasomotor symptoms – the small blood vessels in the skin suddenly widen, your heart rate can rise, and you may feel a wave of intense heat followed by sweating.
From a sleep point of view:
- The heat itself wakes you
- Sweat evaporating on the skin can feel chilly afterwards
- Damp clothing or sheets increase friction on already thinner, drier skin
- Getting up to change, shower or cool down fragments your sleep cycle
Research on sleep and temperature shows that a hotter thermal environment increases wakefulness and reduces deep and REM sleep.
So if you feel as if you have aged ten years in one summer, it is not simply in your head. Poor sleep multiplies daytime fatigue, mood swings, joint pain and brain fog.
Step one – cool the room, not just your face
Australian health agencies emphasise that staying cool and hydrated is the key to reducing heat stress in summer, especially during heatwaves when night time temperatures stay high.
For menopause sleep, that advice comes into your bedroom:
- Aim for a cool bedroom temperature
Sleep and menopause specialists often recommend a bedroom in the mid teens in degrees Celsius, if you have that level of control, to counteract overheating and night sweats. - Use fans and air conditioning strategically
A pedestal fan that moves air across the whole bed is more helpful than a tiny desk fan aimed only at your face. If you have air conditioning, pre-cool the room before bed so the system can work less overnight. - Block and then flush heat
During the day, keep blinds or curtains closed and windows shut if it is hotter outside than in. Open windows once the outdoor temperature drops so the room can release stored heat. - Make your bed like a layered outfit
Instead of one heavy doona, use lighter layers you can peel back. A top sheet plus a light cover is easier to adjust mid flush than wrestling a quilt.
This is not vanity. In prolonged heat, broken sleep and dehydration can push people towards heat related illness, particularly in midlife and beyond.
Step two – choose skin kind textiles
After 40, the outer skin barrier can become drier and thinner, especially if you have gone through radiotherapy, surgical menopause or long term endocrine therapy. That makes rough fabrics and seams feel harsher.
Think about the layers that touch you for eight hours:
- Sleepwear
Natural fibres such as cotton, linen or bamboo breathe and absorb sweat better than many synthetics. Loose cuts prevent cling and friction at the chest, under the breasts, inner thighs and vulval area. - Bedding
If you wake drenched, consider having a second fitted sheet and pillowcase folded at the end of the bed. A quick change is less disruptive than remaking the entire bed. Choose weaves that feel smooth to your skin – sateen or well washed percale, rather than anything scratchy. - Friction zones
Before bed, pat dry carefully after your shower, then apply a simple, fragrance free emollient or barrier cream to areas that tend to rub – under the breasts, under the belly fold, inner thighs and external vulval area. This helps reduce chafing if you sweat repeatedly overnight.
If any product stings or leaves you sore, rinse it off and avoid it. The goal is comfort and barrier support, not a new irritation.

Step three – look at your evening triggers
Not every night sweat can be controlled, but some triggers are worth experimenting with:
- Alcohol and caffeine
Both can worsen vasomotor symptoms and disturb sleep. Health advice for hot weather also recommends limiting these because they contribute to dehydration. - Spicy or very heavy meals late at night
These can make your internal thermostat work harder. Aim for your main hot meal earlier in the evening and something lighter if you are hungry later. - Screen and stress exposure
Blue light, emails and doom scrolling keep your brain in alert mode. Replace the last 30 to 60 minutes on your phone with a predictable wind down ritual – reading, gentle stretching, breathing exercises or a short guided relaxation. - Overheating exercise
Movement is excellent for midlife health, but very intense late evening workouts in hot weather can make it harder to cool down. If possible, schedule vigorous sessions earlier in the day and keep evenings for lighter movement.
None of these adjustments will eliminate hormonal symptoms, but together they can reduce how often you wake and how long it takes you to settle again.
Step four – if you share a bed
This is where men come in as supporting characters.
If your partner is still happily sleeping under the heavy doona while you are flipping the pillow to find a cool patch, you are not alone. Heat comfort is personal.
A practical midlife compromise:
- Separate top layers – two single doonas or a doona plus sheet instead of one shared heavy quilt
- A quiet code for when you need to move to the couch or spare room without anyone taking it personally
- An honest conversation about why you might keep a fan on or a window open, even in January
You can explain it in simple terms:
My internal thermostat is glitchy at the moment. If I need extra air or different bedding, it is about my biology, not about how much I like you.
Sleep is a health issue, not a romance test.
When to talk to a doctor
Night sweats and hot flushes are common in menopause, but they are not the only cause. In some cases, sweating at night can signal infection, endocrine conditions, medication side effects or, rarely, more serious illness.
Book a medical review if:
- Night sweats are new, severe or drenching
- You have fever, weight loss, pain, bleeding or other unexplained symptoms
- Sleep disruption is making it difficult to function, work or drive safely
- You have a history of cancer, heart disease or clotting problems
A GP or menopause trained clinician can help assess whether symptoms are primarily hormonal or whether other investigations are needed. They can also discuss medical options for vasomotor symptoms, as well as non drug strategies, to improve sleep and quality of life.
A kinder way to measure a summer night
It is easy to judge yourself by the clock – how late you got to sleep, how many minutes you were awake, how early the alarm dragged you up.
For this stage of life, a better set of questions might be:
- Did I give my body a fair chance – cool room, breathable fabrics, fewer triggers
- Did I treat my waking moments with kindness, rather than anger
- Did I ask for the changes I needed, rather than silently endure
Summer will always bring hot nights. Menopause adds its own internal weather. You deserve an environment and a routine that work with you, not against you.
Even if you cannot change the temperature outside, you can change the story inside your bedroom from battle to collaboration.
 Part proceeds to McGrath Foundation
Part proceeds to McGrath Foundation